Cystic Fibrosis in Africa
by Hugues Abriel and Patricia Teixidor
What is cystic fibrosis?
Every 4 days, a baby is born with cystic fibrosis.
Cystic Fibrosis (CF) is a rare disease, which means it is found in less than 1 out of 2’000 patients. Since most rare diseases are of genetic origin, they are challenging to diagnose accurately in African countries. We are researching how to diagnose cystic fibrosis more efficiently.
In CF, the gene encoding a chloride ion channel (CFTR) is mutated and does not function properly. This defect causes recurring lung infections and malfunction of the pancreas, leading to the failure to grow in affected children. Life expectancy is reduced in CF patients, and African CF patients usually die before age 20.
What does it mean to live with cystic fibrosis?
Imagine living with an unpredictable disease that forces you to go to the hospital two times per year for 15 days to receive antibiotics and physiotherapy sessions, not knowing what it feels to live a ’normal’ life because you need to take up to 40 tablets per day and nebulized drugs.
We interviewed the mother of an 18-year-old patient of African origin who lives in Switzerland and was diagnosed at age 2. Watch the video below (published with her permission).
Why is research in cystic fibrosis in Africa so important and why do we need your support?
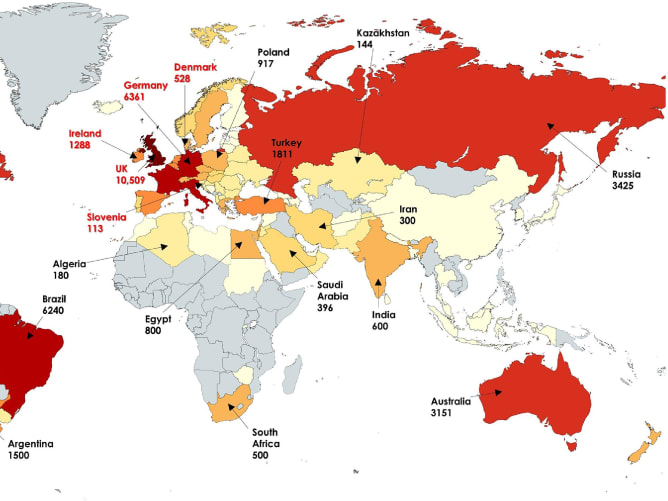
We have realised that CF in Africa is still a mystery. We still do not know how frequent the disease is, diagnosis is a huge challenge, and there are almost no treatments. A paper from 2022 showed that most patients diagnosed with CF are currently from Egypt and South Africa. As shown in the picture, besides these two countries, there is very little information regarding CF in this continent.
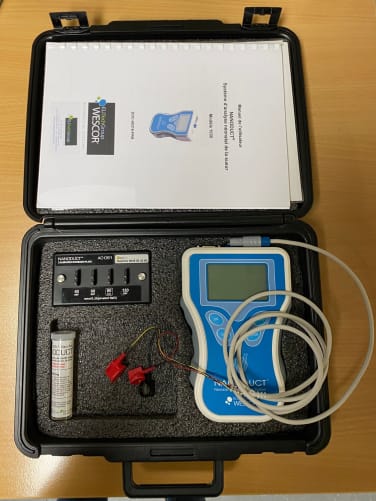
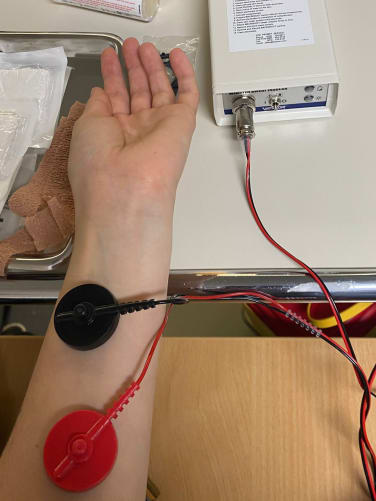
In Switzerland and the rest of the high-income countries, a «sweat test» performed by a Nanoduct® device measures chloride concentration in children’s sweat. If chloride is too high, this is a diagnostic element for cystic fibrosis. However, in Morocco, where Nada is from, only one hospital has such an instrument, and there are very few in Africa.
Nada started working on a nanopore-based approach to sequence CFTR, the gene mutated in CF patients. However, the pediatricians from Fez would need to perform this sweat test to obtain an accurate clinical diagnosis. The gene of these patients would then be sequenced with the new technique that Nada is developing. Michèle is working on her MD thesis about CF and will help Nada to use the machine in Fez.
We started this campaign to purchase this essential device that cost approximately CHF 10’000. For every Swiss franc someone contributes to our science project, the Swiss National Science Foundation will give us another franc, up to CHF 5’000. With the amount we will raise, we can buy a Nanoduct Sweat Test Machine and cover all costs related to Nada and Michèle’s project.
Nada has already obtained preliminary results about mutations that CF patients present in Morocco. You will allow her to enlarge her patient cohort and continue her genetic research by backing us. Research is the key to improving therapeutic options for CF patients. We see this project as a pilot project that could be extended to other African countries, such as the Democratic Republic of the Congo (Kinshasa), where we are also in contact with pediatricians.
This project is a result of the collaboration with the lab of Prof. Laila Bouguenouch from the University hospital in Fez.